
has been a buzzword in the clinical trial industry for the past few years with all the big pharma companies discussing how to put patients at the centre of trials.
This however might not be the best solution, with speakers at , held at the Hyatt Regency Hotel in Barcelona, talking about how mutual benefit is more important.
Mutual benefit in this context refers to ensuring that all parties involved in a clinical trial benefit from research – this means sponsors, sites, patients, patient advocacy groups and CROs, amongst others involved in the development process.
As a result, those at the top need to consider how their trial design benefits parties at all stages of development.
Everyone should benefit
Speaking in a panel about exploring the transition of innovation and technological advancements in clinical trials Upinder Grewal, strategic lead exploration and discovery, DS&AI at Bayer, said that everyone must work together from the very beginning.
“It’s the concept of co-creation,” Grewal explained. “It’s not just coming from one part of the game, we must work together with all the players- that is critical. That comes by understanding the real needs from the very beginning, considering the perspectives of the patients, of the regulators, of the sponsors.”

In the same panel, co-founder of IOMED, an AI healthcare data company, Gabriel Maeztu adds: “The big problem is who is benefiting from this innovation? If that innovation is not getting to all the stakeholders and just one party is getting benefit then the innovation is not felt by everyone equally. That’s a big struggle.”
Maeztu shared an example of how a sponsor used AI to evaluate data in a dermatology study. While the study investigators were initially excited at the concept of using AI when the data was being evaluated, only the sponsors had access, with investigators later asking how they benefitted from participating in that study, which Maeztu said meant those investigators may not be as inclined to work with the sponsor again.
“When one of the stakeholders is not getting direct value from the innovation, when you try to repeat this work is when you get a problem,” Maetzu added.
Amelia Hursey, Parkinson’s research manager for Parkinson’s Europe, held a session about building clinical trials with the perspective of the patients in mind,
Hursey adds that even when parties might be trying to make trials mutually beneficial, there are still barriers in place which exclude certain parties from trials which are simple to fix.

“Even the language used in trials is a huge barrier and that isn’t the different actual language itself but the terminology everyone uses. Mutual investment doesn’t require education, it requires knowledge, wisdom, and the sharing of insights,” said Hursey.
“We do not want to just educate people about what that research is doing but make research with them.”
In another panel discussing how to maximise the , Richard Gray, managing partner of EMEAR Enterprise, Medidata Solutions, said it is important to have an appreciation of the site’s capacity. “You have got to try and have a relationship at a site level. You must think about site burden to support sites in terms of scalability and their operating model.”
When a site investigator shared her experiences in the session, she said sites need better communication, training and tech manuals. Gray acknowledged the challenges sites are facing, adding: “There’s always all this promise of where innovation and advanced technology can take us but unless you solve the fundamental things and get the communication right, you are limited as to where you can go.”
Head of the late phase programme management respiratory and immunology at AstraZeneca, Alina Pszczółkowska, held a session about patient burden.

The pharma giant has created the protocol complexity tool which evaluates trial design and protocol and works out how complex it is for a patient to participate in a bid to make .
The tool, developed using data collected in patient surveys from a variety of AstraZeneca trials, provides a numerical scale which evaluates patient burden considering visit schedule, procedural burden and ePRO experience.
Regulation and tech also at forefront of discussion
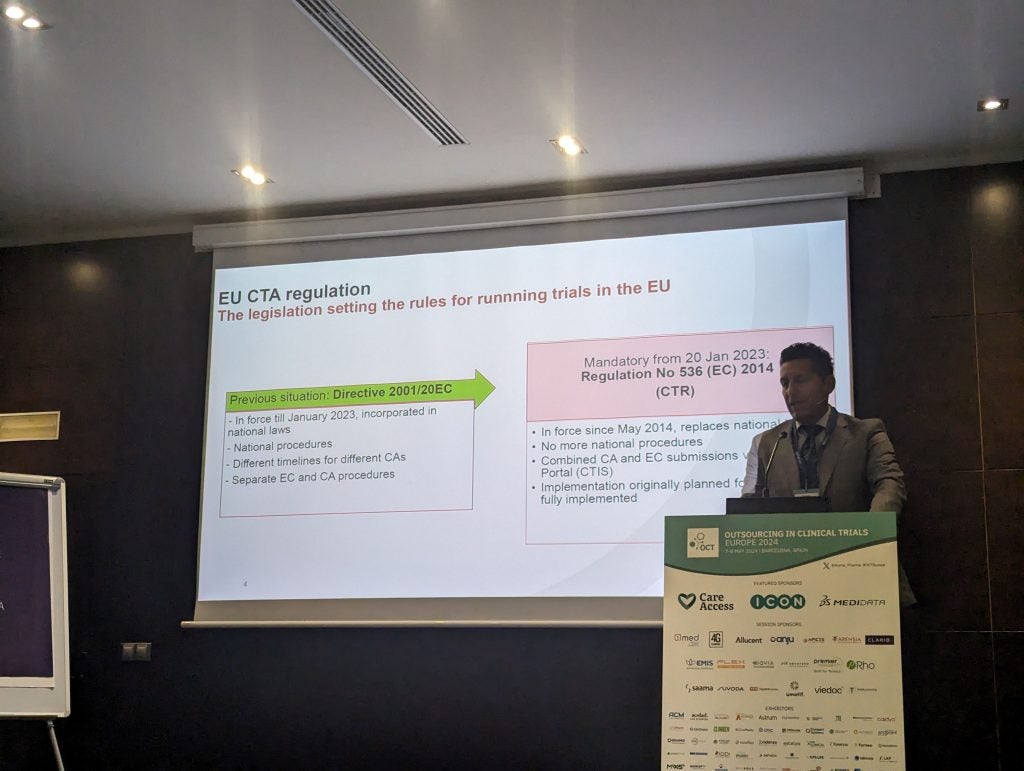
Other sessions at OCT Europe 2024 discussed regulatory changes with the European Medicines Agency’s (EMA) move from the Clinical Trials Directive (CTD) to the Clinical Trials (CTR). By January 2025, sponsors will need to have moved all their trials, including ongoing studies to the CTR.
One of the biggest issues with the which creates complexities when filing in different countries.
Dr Sol Yates, associate director of European regulatory affairs for Shionogi Europe, said: “The issue is not with the CTR, the issue is some health authorities are, unfortunately, making their own interpretations of the regulation. What happens is some countries ask questions which you would not anticipate and questions which other countries do not care about. Certain countries really focus on certain issues and then you may have few other options but to withdraw in that country.”
Another regulatory topic discussed at OCT Europe 2024 was the
Silvia Perez, director of clinical quality compliance at AstraZeneca spoke about the updates made to sections on principles of ICH, investigators, and sponsors.
The biggest change to the guidance was the introduction of a data guidance section in the guidance, providing a great deal of clarity about where responsibility lies.
AI and machine learning were also top of the agenda, with the opening keynote discussing a system called . Archer is a system which automatically transfers electronic health record to electronic data capture (EHR-to-EDC).

Currently, in Europe, investigators will input data collected about a patient in a trial into their EHR as standard of care before transferring this manually to the EDC to provide a sponsor. Archer uses that data from the EHR and automatically transfers this in a deidentified manner to sponsors.
There were also questions asked about the lack of tech development in EMA guidance, with Yates questioned about whether there was any mention of AI in the CTR – which he confirmed there was not. This raised some eyebrows given its increasing prevalence in the data processing field.


